Why the Right Credentialing Contractor Matters
Accurate and Timely Credentialing Results in Higher Revenue
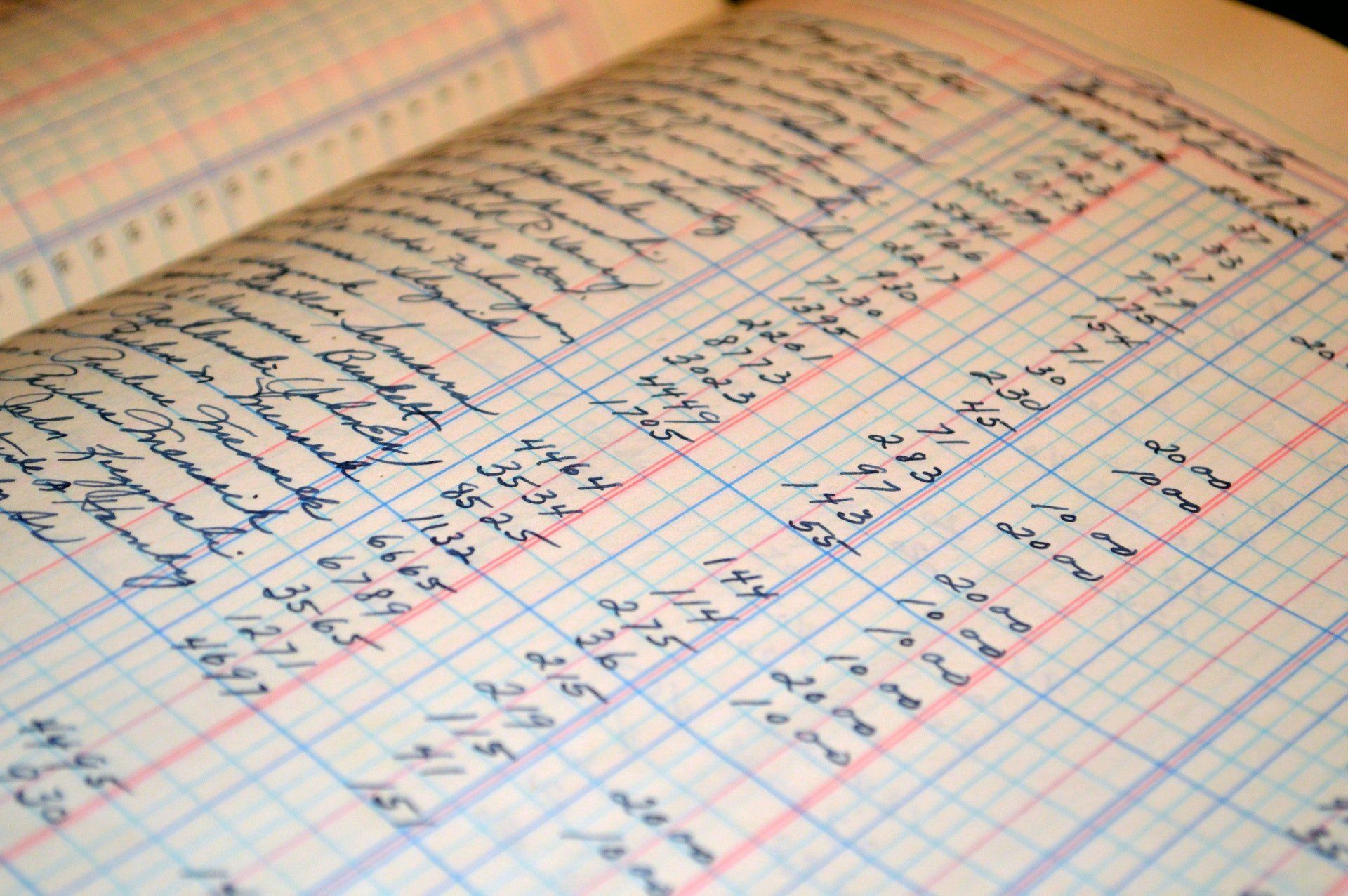
In the realm of healthcare, especially within the domain of behavioral health, the importance of proper credentialing cannot be overstated. It’s the bedrock upon which trust, reliability, and professionalism are established between practitioners and patients. Credentialing is a meticulous process that validates the qualifications, experience, and compliance of healthcare providers, ensuring they meet the necessary standards to deliver quality care. However, the success of this crucial process greatly hinges on partnering with reliable and trustworthy credentialing experts.
The landscape of behavioral health is multifaceted and continually evolving, demanding a meticulous approach to credentialing. Given the complex nature of mental health services, finding the right credentialing contractor becomes paramount. Here’s why their role is indispensable:
Upholding Regulatory Compliance
Navigating the maze of regulatory frameworks, insurance requirements, and compliance standards can be daunting for any healthcare professional. Behavioral health credentialing experts adeptly understand these intricacies, ensuring that providers adhere to the regulatory landscape. Compliance with standards not only mitigates legal risks but also fosters trust among patients and stakeholders.
Streamlining the Credentialing Process
Credentialing can be an arduous process involving extensive paperwork, verifications, and follow-ups. An experienced credentialing contractor brings efficiency by managing the entire process, from initial application to maintaining credentials. This alleviates the administrative burden on providers, enabling them to focus on patient care.
Mitigating Errors and Delays
Errors or delays in the credentialing process can lead to disrupted services, delayed payments, and potential patient dissatisfaction. A competent credentialing contractor meticulously reviews documentation, minimizing errors and ensuring a smoother, expedited process. Timely credentialing helps providers seamlessly integrate into healthcare networks and commence patient care without unnecessary delays.
Securing Reimbursements and Revenue
Accurate credentialing directly impacts a provider’s ability to receive reimbursements from insurance companies and government programs. Reliable credentialing experts ensure that practitioners are enrolled with insurance panels, maximizing their ability to receive timely payments for services rendered. This significantly impacts a provider’s revenue stream and sustainability.
Enhancing Professional Reputation
In the sensitive realm of behavioral health, a provider’s reputation is paramount. Patients seek care from professionals they trust. A credentialing contractor that maintains accuracy and professionalism contributes significantly to building and upholding a provider’s reputation for reliability and expertise.
Conclusion
In the world of behavioral health, the right credentialing contractor is more than a mere service provider; they are an essential partner in a provider’s journey. The intricate nature of mental health services demands precision, reliability, and adherence to stringent standards. A trusted credentialing expert not only ensures compliance but also empowers providers to focus on what matters most—their patients.
Choosing the right credentialing contractor is an investment in a provider’s success and the well-being of their patients. It’s a decision that significantly impacts operational efficiency, financial stability, and the reputation of behavioral health practitioners. Collaborating with a reputable credentialing expert is not just a choice; it’s a strategic imperative for those dedicated to delivering exceptional behavioral health care.
Request a Credentialing Quote
Thanks for reaching out! I'll be in touch as soon as possible.
Please try again later.


Latest news