Demystifying Insurance Paneling
A Guide for New Behavioral Health Providers
As a new behavioral health provider entering the field, navigating the landscape of insurance paneling can be as challenging as it is essential. Understanding the nuances, requirements, and benefits of joining insurance panels is pivotal in establishing a successful practice and ensuring access to a broader clientele. So, let’s delve into what insurance paneling entails and what you should know as a burgeoning professional.
What is Insurance Paneling?
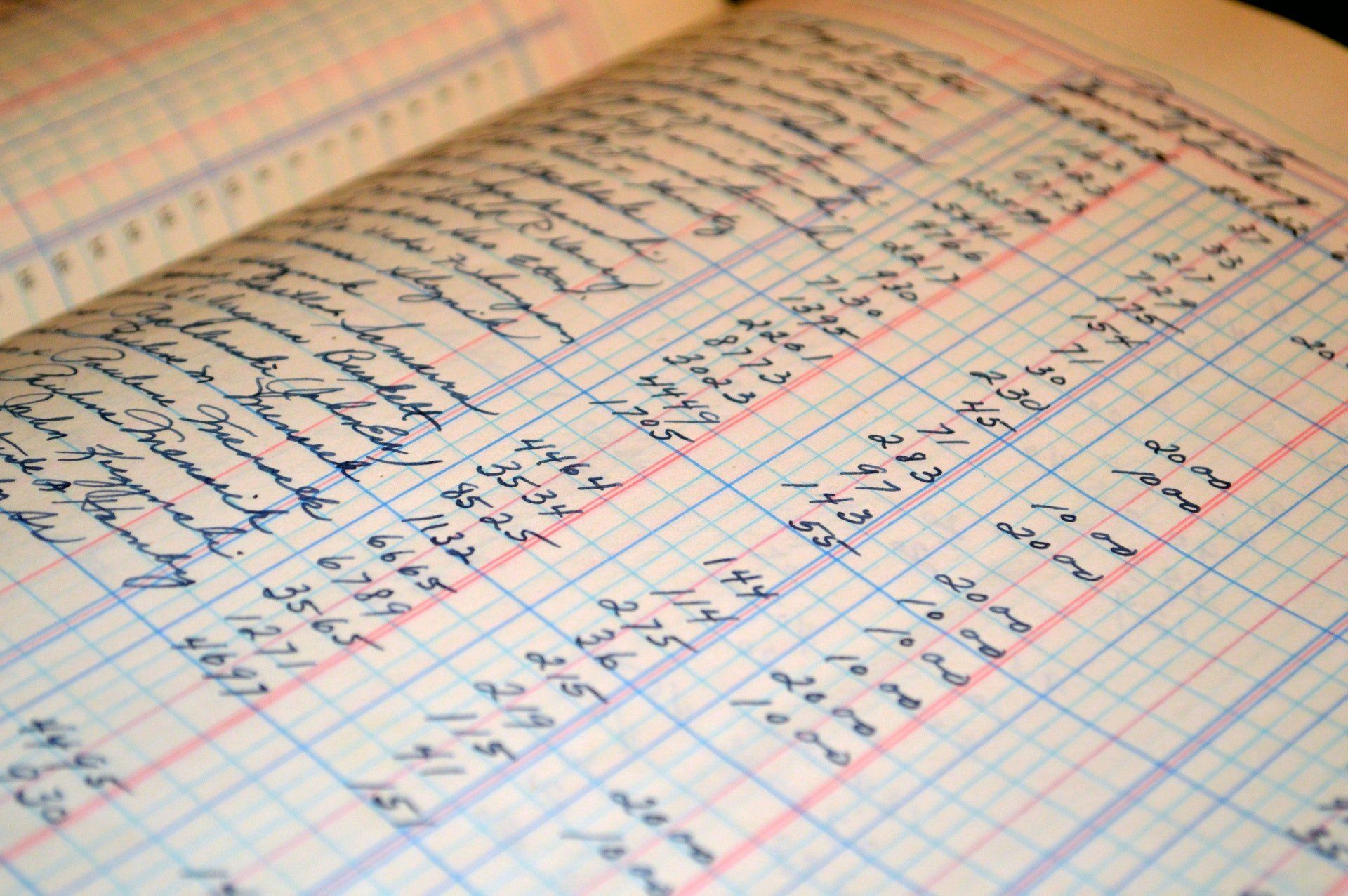
Insurance paneling, also known as credentialing, is when healthcare providers, including behavioral health specialists, become affiliated with specific insurance networks or panels. These panels comprise healthcare professionals who have agreed to provide services to the insurance company's members at predetermined rates.
Why Join an Insurance Panel?
- Expanded Client Base: Joining insurance panels widens your potential client base. Many individuals seek therapy or counseling services covered by their insurance plans, making it more likely for them to choose providers within their network.
- Financial Viability: Being part of insurance panels can ensure a steady stream of clients and a more predictable income flow. This is especially beneficial for new providers establishing their practices.
- Credibility and Trust: Inclusion in insurance panels can enhance your credibility and trustworthiness among potential clients. It implies that you meet specific standards and requirements the insurance company sets.
What You Should Consider:
- Credentialing Process: Each insurance company has its own credentialing process. Expect to undergo a rigorous procedure that involves verifying your education, licensure, and often, clinical experience.
- Contractual Agreements: Review and understand the terms of the contract thoroughly before signing. Pay attention to reimbursement rates, the number of clients you’re expected to serve, and any restrictions or requirements imposed.
- Administrative Workload: Billing, claims submissions, and adhering to specific documentation requirements are part of being an in-network provider. Prepare to manage administrative tasks efficiently or plan on paying a contractor or office manager to help.
- Reimbursement Rates: While being part of an insurance panel provides a steady stream of clients, reimbursement rates can vary. Ensure that the rates are acceptable and sustainable for your practice.
Tips for Navigating Insurance Paneling:
- Research and Select Wisely: Conduct thorough research on different insurance panels and choose those aligned with your practice's values, client demographics, and financial goals.
- Network and Seek Guidance: Connect with experienced colleagues or professional associations to seek guidance and insights into the process. Their experiences can be invaluable.
- Ensure Compliance: Stay updated with regulations and compliance standards set by insurance companies. Failure to comply can lead to delays in reimbursements or termination from the panel.
- Consider a Blend of Options: While being in-network can be beneficial, consider a mix of in-network and out-of-network clients to maintain flexibility in your practice.
In conclusion, becoming a part of insurance panels can significantly impact your practice as a behavioral health provider. The decision should be informed, considering both the professional and financial aspects. While it provides access to a larger clientele and financial stability, it also requires commitment, understanding, and adherence to various protocols. By carefully navigating this process, you can establish a thriving practice while providing crucial services to those in need.
Request a Credentialing Quote